Botulinum toxin treatment of plantar fasciitis, clinical applications of point-of-care ultrasound, and other key topics are presented in the new JBJS Guest Editorial “What’s New
Tag: Physical therapy
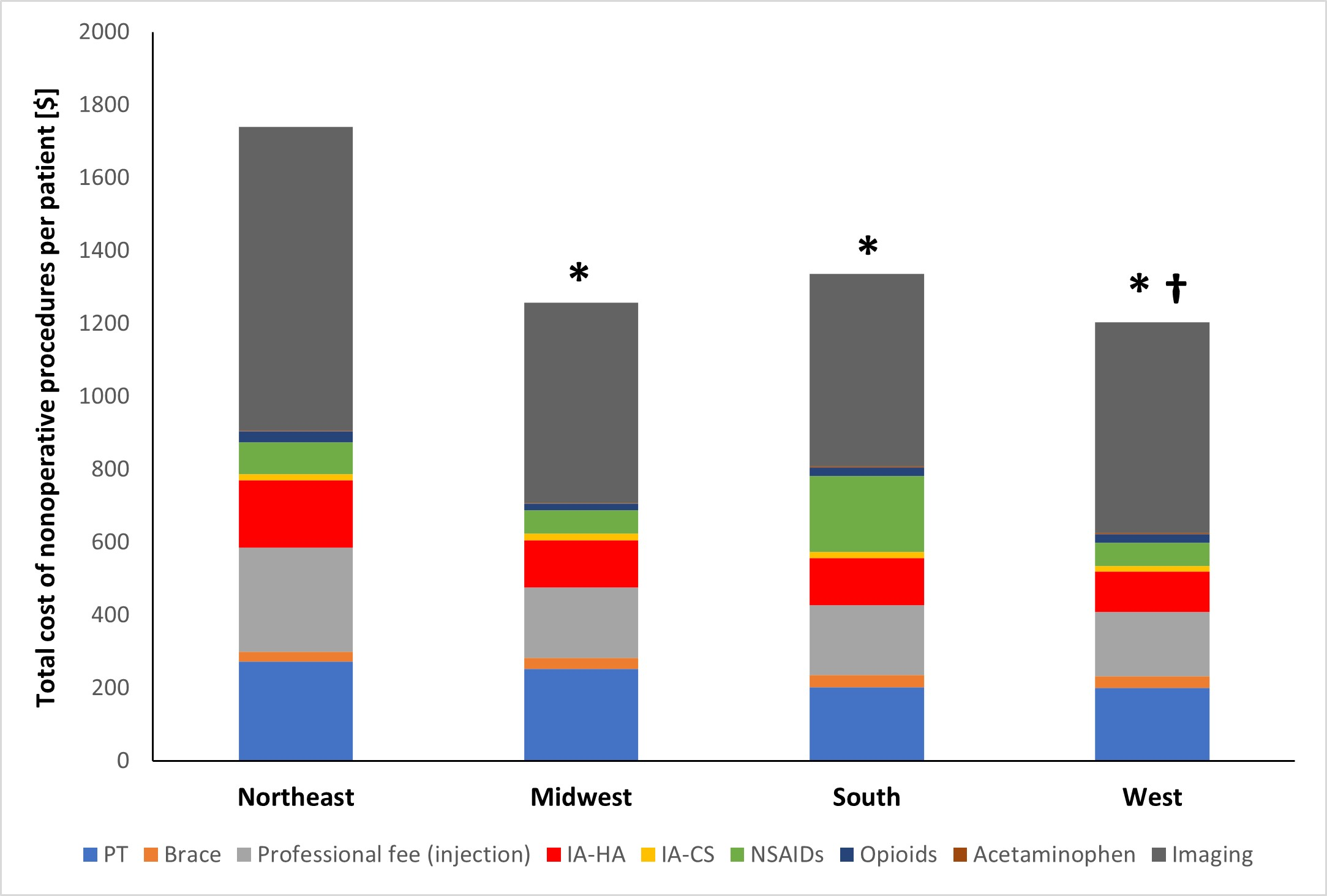
A new JBJS study reviews costs associated with nonoperative management of osteoarthritis in the 1-year period leading up to total knee arthroplasty (TKA). JBJS Deputy
This guest post comes from Jaime Bellamy, DO in response to a recent randomized clinical trial reported in JAMA Network Open and featured in MedPage

Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. This month, co-author

Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. Click here for a collection of all such OrthoBuzz Guest Editorial summaries. This month, co-author Travis
For the last 6 years, JBJS has participated in an “article exchange” collaboration with the Journal of Orthopaedic & Sports Physical Therapy (JOSPT) to support multidisciplinary integration, continuity of
OrthoBuzz occasionally receives posts from guest bloggers. In response to a recent study in The New England Journal of Medicine, the following commentary comes from Jaime L. Bellamy,
OrthoBuzz occasionally receives posts from guest bloggers. In response to a recent study in The Journal of Bone & Joint Surgery, the following commentary comes from Jaime L
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a
OrthoBuzz occasionally receives posts from guest bloggers. In response to a recent study in Arthritis Care & Research, the following commentary comes from Jeffrey B. Stambough, MD.